Even as the cases of Delta variant are on the rise, we know that many people are still reluctant to get the COVID-19 vaccine and that many of you have been trying different approaches with some failures and some successes.
SHSMD members gathered to discuss ways to address vaccination hesitancy in our communities. Inspired by the American Hospital Association (AHA) & Society for Health Care Strategy and Market Development (SHSMD) webinar, Addressing COVID-19 Vaccine Hesitancy in Your Community (available at www.aha.org/joining-hands-greater-impact and YouTube), SHSMD members felt the timing was right to gather and discuss challenges and collaborate on solutions.
The meet up, held on August 2, was facilitated by Alan Shoebridge, director, marketing & communication at Salinas Valley Memorial Healthcare Systems and a member of the SHSMD board. The event welcomed back lead presenters from the July webinar - David Grandy, vice president, and Caroline Franz, system designer, both from Delivery Systems Strategy and Innovation at Kaiser Permanente. After a brief recap on the report, Human Centered Recommendations for Increasing Vaccine Uptake, SHSMD members broke into small groups to share their situations and to collaborate on ideas.
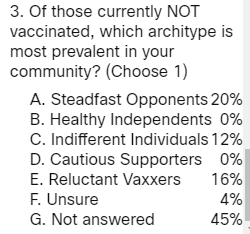
Brief on Demographics
Participants shared their communities, from larger urban areas to small towns all across America. See below for results to three poll questions asked of attendees:
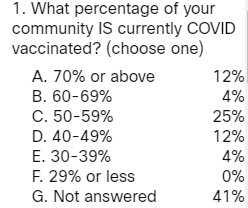
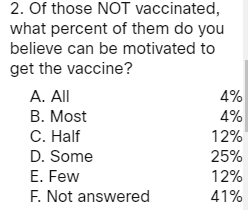
The attendees confirmed that many reasons factor into vaccine hesitancy, based on cultural, political, or social norms and beliefs. Most members reported recent uptick in COVID cases and hospitalizations in their regions.
It is important to address some of the equity barriers affecting systems and communities. For example, requiring valid forms of identification could be a barrier to some.
Here Are Some of Their Stories
A large health system in the southeast with multiple hospitals and over 5,000 employees explained that only 60% of staff were vaccinated, and since other area hospitals have begun to mandate vaccines, it is presumed this organization will also move in that direction. While half of the county’s population is vaccinated, rural areas seem to be lagging at a much lower vaccination rate. Messaging around vaccinations has increased once again since the level of urgency is renewed.
Another organization mentioned that one of the vaccinated leaders of the organization became very sick with COVID and says that it has strengthened his advocacy of vaccination.
In addition, a different organization from Minnesota serving a region that is rural and a college town shared her group felt it is important to prioritize work on addressing risk factors. Rural and military communities are hesitant due to fertility, among other reasons and we need to work together to create persuasive campaigns for their health and public health.
A different group felt that it is important to address barriers that exist in making appointments, so allowing walk-in appointments instead of online registration may help this issue. Addressing cultural stigmas and barriers, like those influencing the Hispanic population is a priority as well as influencing younger generations to get the vaccine within families.
A fourth group shared a few more ideas including:
- Recruiting groups of trusted community members who have influence with others in the community.
- Pivoting messaging with outreach. Not just telling someone to schedule their vaccine or sending them a message on their own, but rather, combining them both. For example, “We know this is scary, we know you have questions. Here are some resources, and if you’re ready to make the step, sign up here.”
- Allowing for walk-ins, making sites open to non-members and providing for primary care visits where vaccination is provided.
- When addressing side effects, providing as many resources as possible and painting the picture of not getting the vaccine and offering up provider resources whenever possible.
Current COVID/Vaccine Related Priorities
Attendees were grouped into virtual breakout rooms and asked each group to report back with three action items and vaccine related priorities.
A key strategy is in sharing stories of patients such the experience of “long haulers” to encourage others to get the vaccine. Sometimes individuals can be reluctant to do so if they fear out lash from those who are on the other side of a heated debate about vaccines. Testimonials from staff are helpful too.
- “FACT vs. FICTION” Campaign
Another attendee shared their larger organization is using a “FACT vs. FICTION” campaign to provide education and data, featuring examples of misinformation such as “I’ve had COVID, so I’m safe” or “I’m young and healthy, so I’ll be able to fight COVID” or “some people get COVID after the vaccine, so what’s the point” coupled with factual explanation. This will be communicated on digital signage for internal staff and in CEO messages. Externally, the campaign will be shared on Facebook and Instagram.
Partnering with physicians is another key strategy since often they are trusted advisors to patients. One organization is partnering with independent physical practices to place ads in local newspapers to encourage vaccinations, which includes branding from multiple providers in the area. It is also important to help physicians with messaging – being careful not to shame others for not getting vaccinated but to gently encourage with facts.
Creating vaccine ambassadors – often physicians but could be pharmacists, nurses, and other specialists and members of the care team. If they are calling patients for other reasons, e.g., time for wellness checkup, then they are being asked to also talk to them about getting vaccinated.
Create handouts in multiple languages – share with caregivers for their outreach efforts to help influence the Hispanic populations, etc.
Making it easy for people to get vaccinated could help those in the “movable middle.” Some organizations have helped make vaccinations available to local businesses, placed booths at the local fair, or partnered with Health Dept to offer a variety of vaccine locations for convenience.
- Letting People Know they are Heard
Listening is important – try to get a sense of the archetypes in your community. One organization is holding small listening sessions starting this month, similar to this SHSMD webinar.
Conclusion
The event was based on the report, Human Centered Recommendations for Increasing Vaccine Uptake, accessible by clicking here. Continue to check www.aha.org/vaccineconfidence for new resources on COVID-19 vaccination efforts.
For anyone unfamiliar with SHSMD, it is a prominent professional membership group for health care strategists and marketers at the American Hospital Association. Getting together to collaboratively address problems and collectively arrive at solutions is just one example of how SHSMD membership can benefit you.
Learning More